Introduction
Aim of Decalcification
Basic Principle
Calcium salts dissolve or bind chemically with specific agents. Proper control of time, temperature, and solution strength prevents tissue damage. Selection of method depends on urgency and diagnostic requirements.
Methods of Decalcification
Laboratories use different approaches depending on tissue type and urgency.
1.Chemical acid method
2.Chelating agent method
3.Ion exchange resin method
4.Electrolytic method
Each method balances speed with preservation quality.
1.Chemical acid method
Simple Mineral Acid
Strong inorganic acids can quickly dissolve calcium. This method is employed in routine laboratories for urgent specimens.
Preparation: The solution is prepared by diluting mineral acids such as hydrochloric or nitric acid, with water serving as the solvent.
Uses: This technique allows for the rapid removal of calcium, facilitates emergency biopsy processing, and is suitable for large bone specimens.
Disadvantages: Potential drawbacks include loss of nuclear staining, damage to cytoplasmic detail, tissue swelling, and inadequate preservation for immunohistochemistry.
Hydrochloric Acid Method
Hydrochloric acid is a well-established decalcifying agent.
Preparation: A 5–10% hydrochloric acid solution can be prepared using distilled water.
Uses: It is effective for rapid decalcification of dense bone and in emergency diagnostic situations.
Disadvantages: It can cause significant tissue damage, may result in poor histological detail, and is not appropriate for delicate specimens.
Nitric Acid Method
Nitric acid provides quick action and slightly improved preservation compared to hydrochloric acid.
Preparation: Dilute 5–10% nitric acid with distilled water.
Uses: Suitable for large bone samples and routine laboratory work that requires efficiency.
Disadvantages: May cause yellow discoloration of tissue, loss of basophilia, and reduced staining quality.
Trichloroacetic Acid
TCA functions as a relatively weak acid with a moderate reaction rate.
Preparation: A solution of 5–10% trichloroacetic acid in distilled water.
Uses: Suitable for small bone fragments and soft calcified tissues.
Disadvantages: Requires a longer fixation time and may cause moderate tissue distortion.
Picric Acid Method
Picric acid functions as a weak acid and a fixative.
Preparation: A saturated aqueous solution of picric acid.
Uses: Suitable for delicate tissues and the preservation of cellular detail.
Disadvantages: Slow decalcification process, explosive properties when dry, and causes yellow staining of tissue.
Formic Acid Method
Formic acid provides an excellent balance between speed and tissue preservation.
Preparation: 5–10% formic acid in distilled water or buffered solution.
Uses: Routine histopathology.Bone marrow biopsies.Specimens requiring good morphology
Disadvantages: Longer processing time.Frequent solution change required.
2. Chelating Agent Method
principle
The chelating agent method eliminates calcium from calcified tissues by binding to calcium ions instead of dissolving them. The primary chelating agent employed is EDTA (Ethylenediaminetetraacetic acid). EDTA creates a stable, soluble complex with calcium ions, which gradually extracts calcium from the tissue without harming cellular structures.
Procedure
Advantages:
Disadvantages:
Uses:
3. Ion Exchange Resin Method
principle
The ion exchange resin method is an adapted version of acid decalcification aimed at enhancing tissue preservation. In this process, an ion exchange resin is incorporated into the decalcifying solution. The resin extracts calcium ions from the solution as they are released from the tissue. This ongoing removal of calcium ions propels the reaction forward, facilitating a quicker and more effective decalcification while maintaining the acid concentration.
Advantages:
Quicker than using the acid method alone. Improved preservation of tissue structure. Decreased damage to cellular detail. Reduced risk of over-decalcification.
Disadvantages:
Higher cost compared to the routine acid method. Requires careful handling of resin. Not available in all laboratories.
Uses:
Small bone biopsies. Specimens that need good histological detail.
4.Electronic Decalcification
Principle
Electronic, or electrolytic decalcification, is a method utilized to remove calcium salts from calcified tissues like bone and teeth. This technique employs an electric current to promote the movement of calcium ions out of the tissue, thus reducing the decalcification time in comparison to traditional methods. When an electric current flows through a decalcifying solution, calcium ions move toward the negative electrode (cathode). This process facilitates the removal of calcium from the tissue immersed in the solution, leading to a quicker decalcification that does not depend solely on chemical reactions.
Procedure
The calcified tissue is adequately fixed, typically in formalin.The specimen is placed in an appropriate decalcifying solution, usually formic acid.Electrodes are positioned in the solution, ensuring the tissue is situated between them.A controlled electric current is applied,causing calcium ions to move toward the cathode and exit the tissue.The process is closely monitored to avoid tissue damage.
Advantages
Rapid decalcification process. Beneficial for urgent diagnostic needs. Decreases overall processing time. Applicable for hard tissues.
Disadvantages
Potential for tissue damage if current regulation is inadequate. Possible reduction in nuclear staining and enzyme activity. Requires specialized equipment. Not intended for routine applications.
Uses
Emergency bone biopsies. Cases needing prompt histopathological diagnosis. Research laboratories.
Affecting Factors
Neutralization Process
Residual acid can harm tissue and affect staining outcomes. Neutralization eliminates excess acid following decalcification. There are several methods of neutralization, including washing in running water and using alkaline solutions such as lithium carbonate or sodium bicarbonate. This process helps restore tissue pH and enhances the quality of staining.
End-Point Determination
Determining completion prevents unnecessary processing.
Radiological Method: X-ray imaging verifies the absence of calcium. This method is highly accurate but necessitates specialized equipment.
Physical Method:Testing the softness of tissue through bending or probing can indicate consistency. However, this method carries a risk of damaging the tissue and is often unreliable.
Chemical Method: Detecting calcium in solution confirms completion. The ammonium oxalate test identifies any residual calcium ions.
Accurate end-point detection is essential for maintaining optimal histological quality. Decalcification should cease immediately once calcium removal is complete.
Errors in Decalcification
Importance in Diagnostic Pathology
Laboratory Safety Considerations
Disclaimer
This article provides general guidance on Biomedical Waste management for educational purposes. Always follow institutional safety protocols, government regulations, and professional training guidelines for handling and disposing of biomedical waste.
Frequently Asked Questions
1. Which is the best agent for preserving tissue morphology?
EDTA provides the best preservation of cellular and nuclear detail.
2. Why is neutralization required after acid decalcification?
Neutralization removes residual acid and improves staining quality.
3. Which method gives the fastest result?
Strong mineral acids provide the fastest results but damage tissue.
Written by Jambir Sk Certified Medical Laboratory Technologist
Disclaimer: This content is for educational purposes only and should not be consideredas medical advice. Always consult a qualified doctor.We do not provide professional medical advice, diagnosis, or treatment.All health-related content is based on research, knowledge, and general awareness.Always consult a licensed healthcare provider for any medical concerns.HealthSeba.com will not be responsible for any loss, harm, or damage caused by the use of information available on this site.
Related Posts
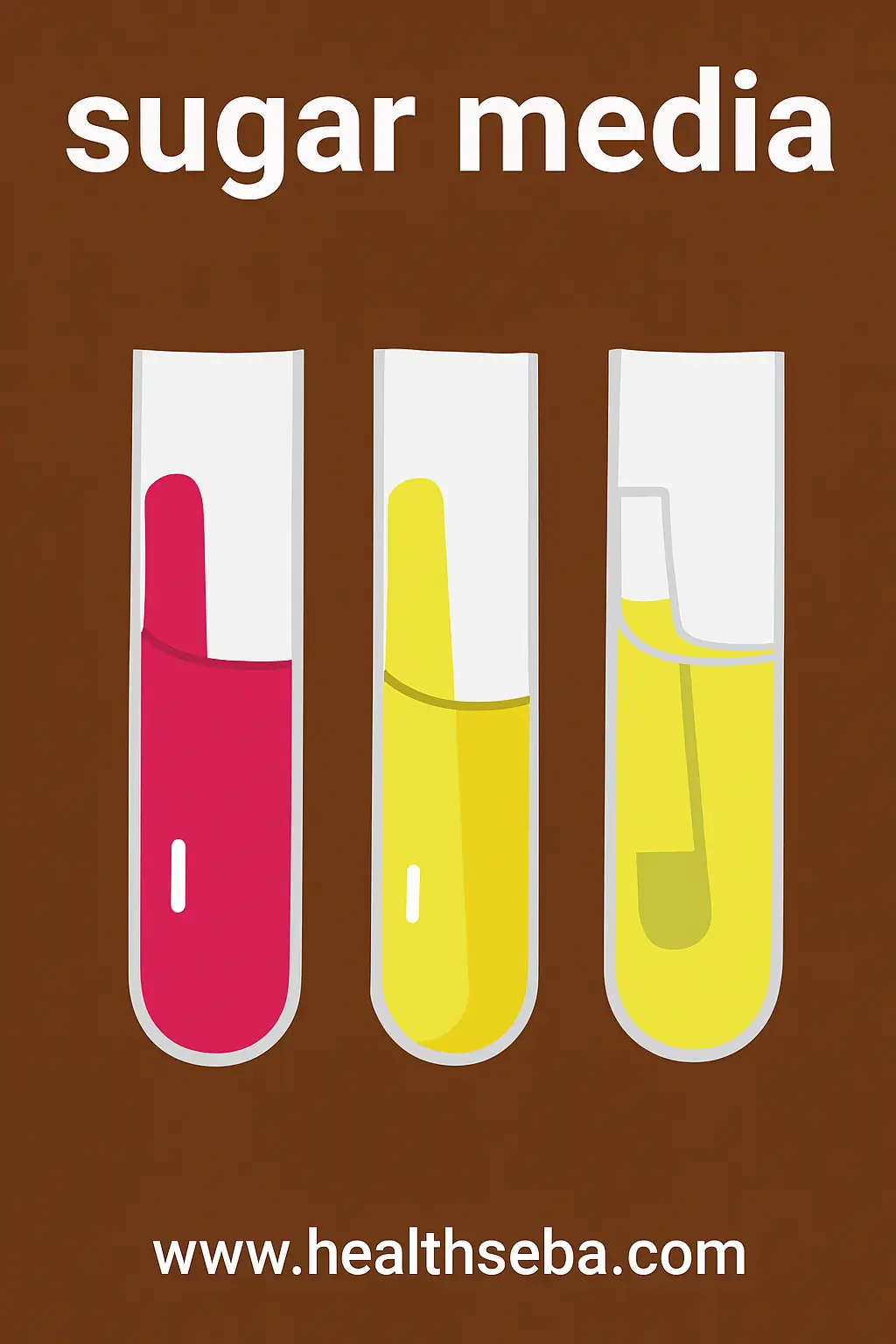
Sugar Media Composition Preparation Uses
Introduction Sugar media are specialized differential culture media used in…
Instrumental Hazards
Introduction A Clinical Biochemistry Laboratory supports modern diagnosis by analyzing…